DISCOVERIES REPORTS (ISSN 2393249X), 2021, volume 4
Access FULL text of the manuscript here: Full text (PDF)
CITATION: Haq AU, Bashir I, Ikhlaq A, Arshad AR, Ijaz F, Haq AU, Aftab RK. A Systematic Review of COVID-19 Reinfections. Discoveries Reports, 2021; 4: e21. DOI: 10.15190/drep.2021.6 Submitted: Jan 1, 2021; Revised: April 5, 2021; Accepted: April 23, 2021; Published: June 30, 2021;
A Systematic Review of COVID-19 Reinfections
Aizaz Ul Haq (1), Imtiaz Bashir (2), Azal Ikhlaq (2), Abdul Rehman Arshad (2), Farhat Ijaz (3,*), Anwar Ul Haq (4), Rana Khurram Aftab (5)
(1) Akhtar Saeed Medical College, Lahore. Pakistan
(2) CMH Lahore Medical College and Institute of Dentistry, Lahore, Pakistan
(3) Department of Physiology, CMH Lahore Medical College and Institute of Dentistry, Lahore, Pakistan
(4) Lahore General Hospital, Lahore, Pakistan
(5) Punjab Institute of Cardiology, Lahore, Pakistan
* Corresponding author: Dr. Farhat Ijaz, MBBS, MPhil.Assistant Professor, Department of Physiology,CMH Lahore Medical College and Institute of Dentistry, Lahore, Pakistan. Email: farhat_khurram_rana@cmhlahore.edu.pk
Abstract
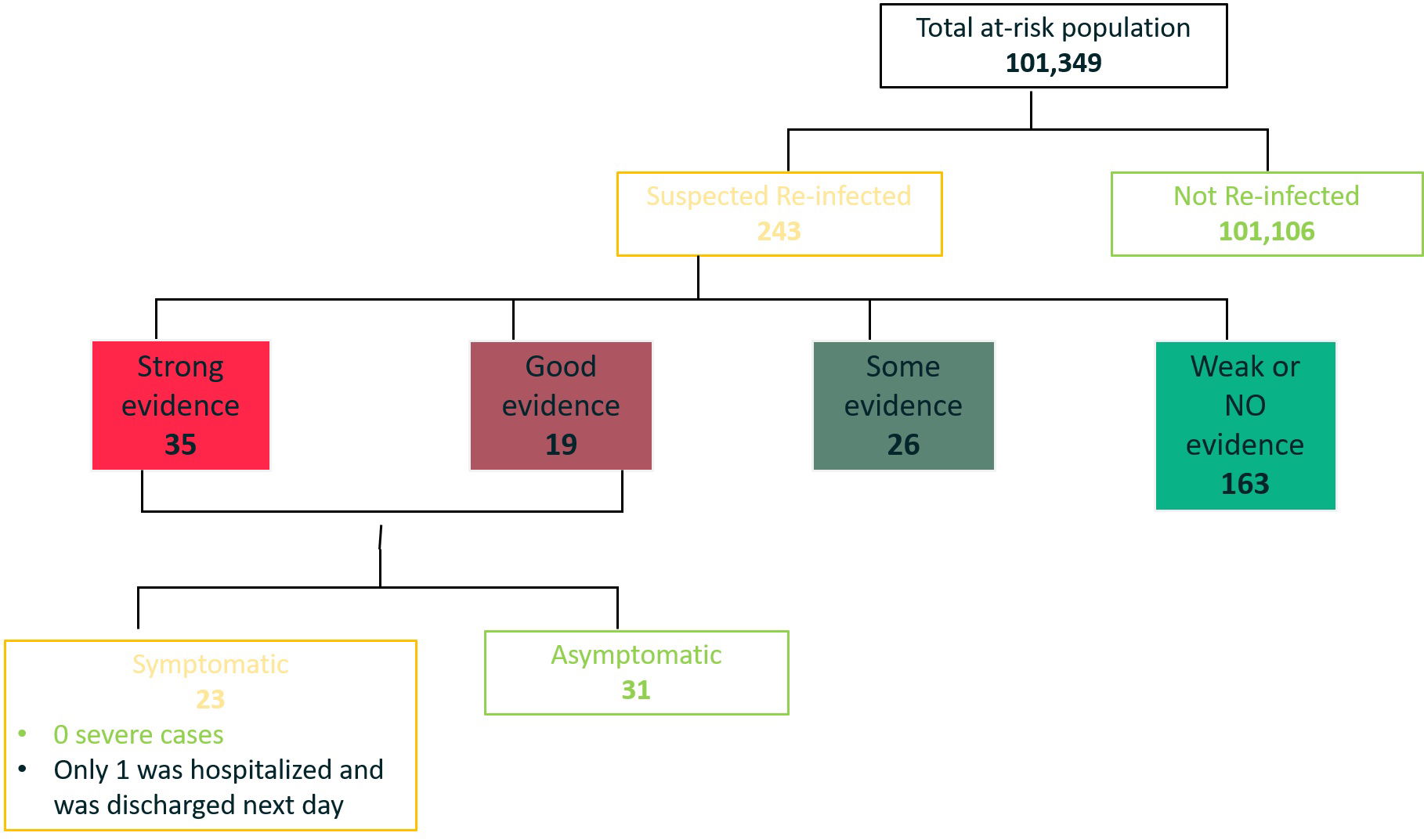
The In this review, we have summarized available data on SARS-CoV-2 reinfection and discussed the possible explanations for this phe-nomenon. A systematic review of literature was conducted concluding that although rare, COVID-19 reinfections are indeed possible, generally tend to occur in immunocompromised individuals and frequently involve a new variant strain of the SARS-CoV-2 virus. We suggest that this may be due to re-exposure, co-infections, or prolonged viral shedding due to a known or unknown etiology. We think that the criteria for classifying COVID-19 infection as a reinfection should be revised, such that either there is genomic evidence of infection with a different strain or there should be a 90 day ‘indefinite period’ time interval between the first and second COVID-19 infection, to avoid confusion with prolonged shedding of the virus.
References
1. Coronavirus Cases. [Accessed: May 17, 2021]. https://www.worldometers.info/coronavirus/
2. Iwasaki A. What reinfections mean for COVID-19. The Lancet Infectious Diseases. 2020 Oct 12.
3. Findings from investigation and analysis of re-positive cases. [Accessed: Jan 2, 2021]. http://www.kdca.go.kr/board/board.es?mid=a30402000000&bid=0030&act=view&list_no=367267&nPage=24
4. Paz-Bailey G, Rosenberg ES, Sharp TM. Persistence of Zika virus in body fluids. The New England journal of medicine. 2019 Jan 10;380(2):198.
5. Oh MD, Park WB, Choe PG, Choi SJ, Kim JI, Chae J, Park SS, Kim EC, Oh HS, Kim EJ, Nam EY. Viral load kinetics of MERS coronavirus infection. New England Journal of Medicine. 2016 Sep 29;375(13):1303-5.
6. Wang Y, Guo Q, Yan Z, Zhou D, Zhang W, Zhou S, Li YP, Yuan J, Uyeki TM, Shen X, Wu W. Factors associated with prolonged viral shedding in patients with avian influenza A (H7N9) virus infection. The Journal of infectious diseases. 2018;217(11):1708-17.
7. Centers for Disease Control and Prevention. Interim Guidance on Ending Isolation and Precautions for Adults with COVID-19. [Accessed: Jan 2, 2021] https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html
8. European Centre for Disease Prevention and Control E. Reinfection with SARS-CoV-2: considerations for public health response. 2020. https://www.ecdc.europa.eu/sites/default/files/documents/Re-infection-and-viral-shedding-threat-assessment-brief.pdf
9. Nachmias V, Fusman R, Mann S, Koren G. The first case of documented Covid-19 reinfection in Israel. IDCases. 2020 Jan 1;22:e00970.
10. Duggan NM, Ludy SM, Shannon BC, Reisner AT, Wilcox SR. A case report of possible novel coronavirus 2019 reinfection. The American journal of emergency medicine. 2020 Jul 4.
11. Tillett RL, Sevinsky JR, Hartley PD, Kerwin H, Crawford N, Gorzalski A, Laverdure C, Verma SC, Rossetto CC, Jackson D, Farrell MJ. Genomic evidence for reinfection with SARS-CoV-2: a case study. The Lancet Infectious Diseases. 2020 Oct 12.
12. Van Elslande J, Vermeersch P, Vandervoort K, Wawina-Bokalanga T, Vanmechelen B, Wollants E, Laenen L, André E, Van Ranst M, Lagrou K, Maes P. Symptomatic SARS-CoV-2 reinfection by a phylogenetically distinct strain. Clin Infect Dis. 2020 Sep 5.
13. To KK, Hung IF, Ip JD, Chu AW, Chan WM, Tam AR, Fong CH, Yuan S, Tsoi HW, Ng AC, Lee LL. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clinical infectious diseases. 2020 Aug 25.
14. Prado-Vivar B, Becerra-Wong M, Guadalupe JJ, Marquez S, Gutierrez B, Rojas-Silva P, Grunauer M, Trueba G, Barragan V, Cardenas P. COVID-19 Re-Infection by a Phylogenetically Distinct SARS-CoV-2 Variant, First Confirmed Event in South America. First Confirmed Event in South America (September 3, 2020). 2020 Sep 3.
15. Gupta V, Bhoyar RC, Jain A, Srivastava S, Upadhayay R, Imran M, Jolly B, Divakar MK, Sharma D, Sehgal P, Ranjan G. Asymptomatic reinfection in 2 healthcare workers from India with genetically distinct severe acute respiratory syndrome Coronavirus 2. Clinical Infectious Diseases. 2020.
16. Hanif M, Haider MA, Ali MJ, Naz S, Sundas FN. Reinfection of COVID-19 in Pakistan: A First Case Report. Cureus. 2020 Oct;12(10).
17. Islam MJ, Ahmed JU, Haque IU. Reinfection of SARS-CoV-2: reports of three cases from a tertiary care hospital of Bangladesh. BIRDEM Medical Journal. 2020 Dec 28:107-10.
18. Cao H, Ruan L, Liu J, Liao W. The clinical characteristic of eight patients of COVID‐19 with positive RT‐PCR test after discharge. Journal of Medical Virology. 2020; 92(10):2159-2164.
19. Lafaie L, Célarier T, Goethals L, Pozzetto B, Grange S, Ojardias E, Annweiler C, Botelho‐Nevers E. Recurrence or relapse of COVID‐19 in older patients: a description of three cases. Journal of the American Geriatrics Society. 2020 Oct;68(10):2179-83.
20. Dou C, Xie X, Peng Z, Tang H, Jiang Z, Zhong Z, Tang J. A case presentation for positive SARS-CoV-2 RNA recurrence in a patient with a history of type 2 diabetes that had recovered from severe COVID-19. diabetes research and clinical practice. 2020 Aug 1;166:108300.
21. Bonifácio LP, Pereira AP, Balbão VD, Fonseca BA, Passos AD, Bellissimo-Rodrigues F. Are SARS-CoV-2 reinfection and Covid-19 recurrence possible? a case report from Brazil. Revista da Sociedade Brasileira de Medicina Tropical. 2020;53.
22. Selvaraj V, Herman K, Dapaah-Afriyie K. Severe, Symptomatic Reinfection in a Patient with COVID-19. RI Med J (2013). 2020 Nov 9;103:24-6.
23. Abu-Raddad LJ, Chemaitelly H, Malek JA, Ahmed AA, Mohamoud YA, Younuskunju S et al. Assessment of the risk of SARS-CoV-2 reinfection in an intense re-exposure setting. Clin Infect Dis. 2020 Dec 14:ciaa1846.
24. Mumoli N, Vitale J, Mazzone A. Clinical immunity in discharged medical patients with COVID-19. International Journal of Infectious Diseases. 2020 Oct 1;99:229-30.
25. Edridge AW, Kaczorowska J, Hoste AC, Bakker M, Klein M, Loens K, Jebbink MF, Matser A, Kinsella CM, Rueda P, Ieven M. Seasonal coronavirus protective immunity is short-lasting. Nature medicine. 2020 Nov;26(11):1691-3.
26. Deng W, Bao L, Liu J, Xiao C, Liu J, Xue J, Lv Q, Qi F, Gao H, Yu P, Xu Y. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020 Aug 14;369(6505):818-23.
27. Elrashdy F, Aljaddawi AA, Redwan EM, Uversky VN. On the potential role of exosomes in the COVID-19 reinfection/reactivation opportunity. Journal of Biomolecular Structure and Dynamics. 2020 Jul 8:1-2.
28. Addetia A, Crawford KH, Dingens A, Zhu H, Roychoudhury P, Huang ML, Jerome KR, Bloom JD, Greninger AL. Neutralizing antibodies correlate with protection from SARS-CoV-2 in humans during a fishery vessel outbreak with a high attack rate. Journal of clinical microbiology. 2020 Oct 21;58(11).
29. VanBlargan LA, Goo L, Pierson TC. Deconstructing the antiviral neutralizing-antibody response: implications for vaccine development and immunity. Microbiology and Molecular Biology Reviews. 2016 Dec 1;80(4):989-1010.
30. Ma H, Zhao D, Zeng W, Yang Y, Hu X, Zhou P et al. Decline of SARS-CoV-2-specific IgG, IgM and IgA in convalescent COVID-19 patients within 100 days after hospital discharge. Science China Life Sciences. 2020 Aug 28:1-4.
31. Janeway CA Jr, Travers P, Walport M, et al. Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; 2001. Immunological Memory. https://www.ncbi.nlm.nih.gov/books/NBK27158/
32. Dan JM, Mateus J, Kato Y, Hastie KM, Faliti C, Ramirez SI et al. Immunological memory to SARS-CoV-2 assessed for greater than six months after infection. BioRxiv. 2020 Jan 1.
33. Freiborst J, Ogra PL. Mucosal immunity and viral infections. Annals of medicine. 2001 Jan 1;33(3):172-7.
34. Russell MW, Moldoveanu Z, Ogra PL, Mestecky J. Mucosal immunity in COVID-19: A neglected but critical aspect of SARS-CoV-2 infection. Frontiers in Immunology. 2020 Nov 30;11:3221