DISCOVERIES REPORTS (ISSN 2393249X), 2025, volume 8
ORIGINAL ARTICLE
ACCEPTED
CITATION: Hameed MA, Zahra Q, Hameed F. Giant Isolated Splenic Hydatid Cyst with Multiorgan Compression and Pressure-related Atrophy of the Left Hepatic Lobe: A Case Report. Discoveries Reports 2026, 9: eXX. DOI: 10.15190/drep.2026.2
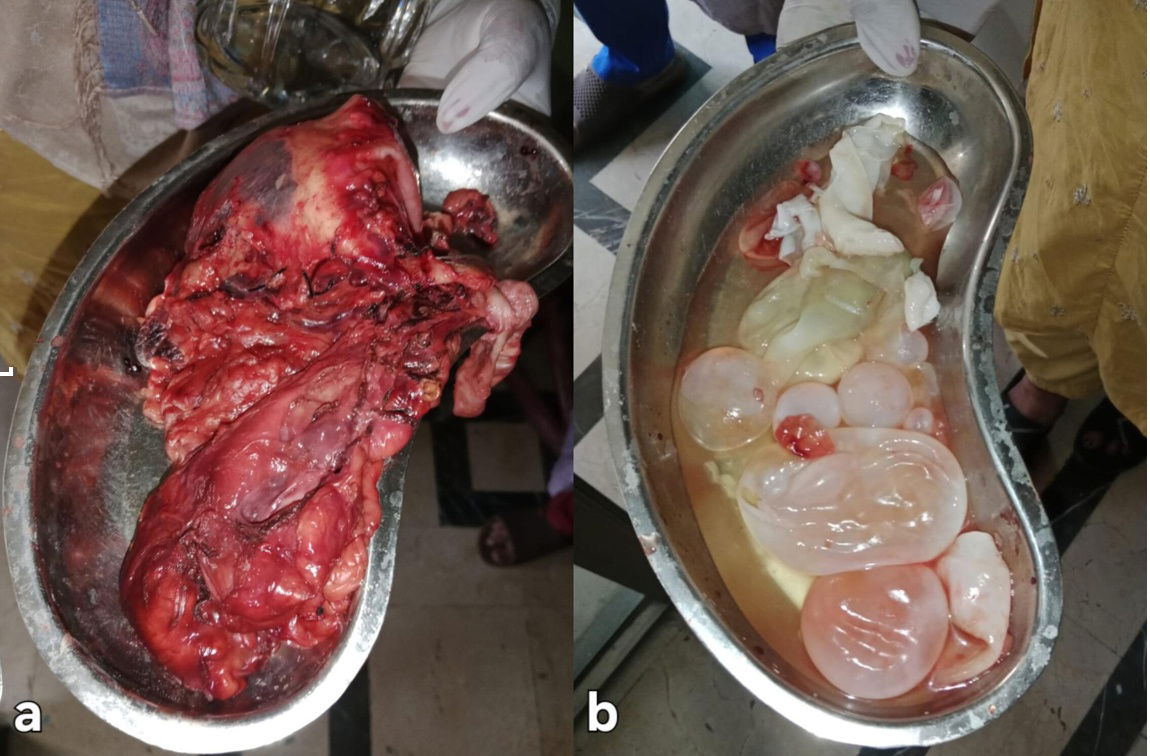
Giant Isolated Splenic Hydatid Cyst with Multiorgan Compression and Pressure-related Atrophy of the Left Hepatic Lobe: A Case Report
Mohammad Abdullah Hameed1*, Qateen Zahra2, Fakhar Hameed3
1 CMH Lahore Medical College & Institute of Dentistry, Lahore, Pakistan
2 Shalamar Medical and Dental College, Lahore, Pakistan
3 Professors Hospital, Faisalabad, Pakistan
* Corresponding author: Mohammad Abdullah Hameed, CMH Lahore Medical College & Institute of Dentistry, Lahore, Pakistan; Email: abdullahfakhar1234@gmail.com.
Abstract
Coming soon.
Access FULL text of the manuscript here: FULL ARTICLE (PDF) - ACCEPTED, NOT YET PUBLISHED
REFERENCES
2. Gottstein B, Reichen J. Hydatid lung disease (echinococcosis/hydatidosis). Clin Chest Med. 2002;23(2):397–408. doi:10.1016/s0272-5231(02)00007-2
3. Zhang W, Zhang Z, Wu W, et al. Epidemiology and control of echinococcosis in central Asia, with particular reference to the People’s Republic of China. Acta Trop. 2015;141(Pt B):235–43. doi:10.1016/j.actatropica.2014.03.014
5. Humphreys WG, Johnston GW. Splenic cysts: a review of 6 cases. Br J Surg. 1979;66(6):407–8. doi:10.1002/bjs.1800660610
6. Malik AA, ul Bari S, Younis M, Wani KA, Rather AA, et al. Primary splenic hydatidosis. Indian J Gastroenterol. 2011;30(4):175–7. doi:10.1007/s12664-011-0104-x
7. Korkut E, Aksungur N, Öztürk G. A retrospective evaluation of spleen hydatid cyst treatments: the spleen-preserving conservative approach is preferable to splenectomy. Eurasian J Med. 2022;54(2):133–7. doi:10.5152/eurasianjmed.2022.20367
8. Rasheed K, Zargar SA, Telwani AA. Hydatid cyst of spleen: a diagnostic challenge. North Am J Med Sci. 2013;5(1):10–20. doi:10.4103/1947-2714.106184
9. Pukar MM, Pukar SM. Giant solitary hydatid cyst of spleen: a case report. Int J Surg Case Rep. 2013;4(4):435–7. doi:10.1016/j.ijscr.2012.12.019
10. Meimarakis G, Grigolia G, Loehe F, et al. Surgical management of splenic echinococcal disease. Eur J Med Res. 2009;14(4):165–72. doi:10.1186/2047-783x-14-4-165
11. WHO Informal Working Group on Echinococcosis. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85(2):253–61. doi:10.1016/S0001-706X(02)00223-1
12. Kaya B, Uçtum Y, Kutanış R. Splenic hydatid cyst attacking retroperitoneum. Turkiye Parazitol Derg. 2010;34(4):254–7. doi:10.5152/tpd.2010.12
13. Milosavljevic V, Veselinovic M, Tadic B, et al. Laparoscopic management of initially unrecognized splenic hydatid cysts: a case report and review of the literature. Medicina (Kaunas). 2019;55(12):771. doi:10.3390/medicina55120771
14. Hariri BA, Haider V, Islam M, et al. Unusual isolated splenic hydatid cyst: a case report. Med Rep. 2024;5:100056. doi:10.1016/j.hmedic.2024.100056
15. Golmohammadzadeh H, Maddah G, Shams Hojjati Y, Abdollahi A, Shabahang H. Splenic cysts: analysis of 16 cases. Casp J Intern Med. 2016;7(3):217–21.
16. Dudhe S, Nimodia D, Mishra GV, Parihar PH, Bhangale P, Kumari A, et al. Isolated splenic involvement in hydatid disease: a case report. Radiol Case Rep. 2025;20(4):1975–8. doi:10.1016/j.radcr.2025.01.033
17. Belli S, Akbulut S, Erbay G, et al. Spontaneous giant splenic hydatid cyst rupture causing fatal anaphylactic shock: a case report and brief literature review. Turk J Gastroenterol. 2014;25(5):527–32. doi:10.5152/tjg.2014.3521
18. Ghabisha S, Ahmed F, Al-wageeh S, et al. Isolated giant primary splenic hydatid cyst in a 10-year-old boy: a case report. Pediatr Health Med Ther. 2021;12:295–300. doi:10.2147/phmt.s295280
19. Lukman K, Sulthana BAAS, Budiman D, et al. Giant splenic cyst: a case series of rare and challenging cases from the last 22 years. Int J Surg Case Rep. 2023;109:108263. doi:10.1016/j.ijscr.2023.108263
20. Karabulut K, Ozden I, Poyanli A, et al. Hepatic atrophy-hypertrophy complex due to Echinococcus granulosus. J Gastrointest Surg. 2006;10(9):1301–5. doi:10.1016/j.gassur.2005.06.007
21. Wake T, Tateishi R, Fukumoto T, Nakagomi R, Kinoshita MN, Nakatsuka T, et al. Improved liver function in patients with cirrhosis due to chronic hepatitis C virus who achieve sustained virologic response is not accompanied by increased liver volume. PLoS One. 2020;15(4):e0231836. doi:10.1371/journal.pone.0231836